A Guide to Home-Based COVID Treatment
- News
-
Nov 10
- Share post
Step-By-Step Doctors’ Plan That Could Save Your Life
Introduction to a guide to home-based covid treatment
A Guide to Home-Based COVID Treatment is built on the rapidly accumulating peer-reviewed published medical research, written by practicing physicians with decades of experience treating patients with all kinds of illnesses.
We provide a step-by-step guide to medically sound early treatments that have a reasonable probability of success in this emergency pandemic. There are oral medications that are approved for other conditions, but not yet proven to be efficacious specifically for COVID-19 by the U.S. Food and Drug Administration. In the global pandemic emergency, large scale randomized clinical trials have not been feasible in the face of such critical illness. The National Institutes of Health at this time does not recommend treatment outside of the hospital because there are no current medications specifically approved for outpatient COVID-19 treatment, even though the mortality rate once patients require hospitalization is unacceptably high.
Thus, treatment administered outside of the hospitalized setting should be under the supervision of a physician or licensed medical professional who is knowledgeable in the use of the medications and the monitoring approach for ambulatory, home-based COVID-19 as described in this guide. Patients who worsen in any way should seek emergency room evaluation immediately.
There are four major pillars to infectious disease pandemic response:
- Contagion control (stop the spread of the virus)
- Early ambulatory, home-based treatment
- Late-stage treatment in hospital
- Vaccination
This guide will focus on the pillar of early, ambulatory, home-based medical treatment overseen by your physician, using a combination of available medicines, already FDA-approved for other medical conditions, and widely used in clinical medicine every day.

We have learned more about what medicines work, how to use them, when to use them, who is most at risk, and what strategies work. Please read this with an open mind. We are writing this to HELP you, to TEACH you how to work with your doctor.
As physicians, we know we need to focus now on early treatment to as the most immediate way to reduce hospitalizations and death. This is your guide to help you know your options, and to use with your personal physician.
Let’s get started!
Chapter 1 of a guide to home-based covid treatment
Overview: SARS-CoV-2 Coronavirus
What Is Coronavirus?
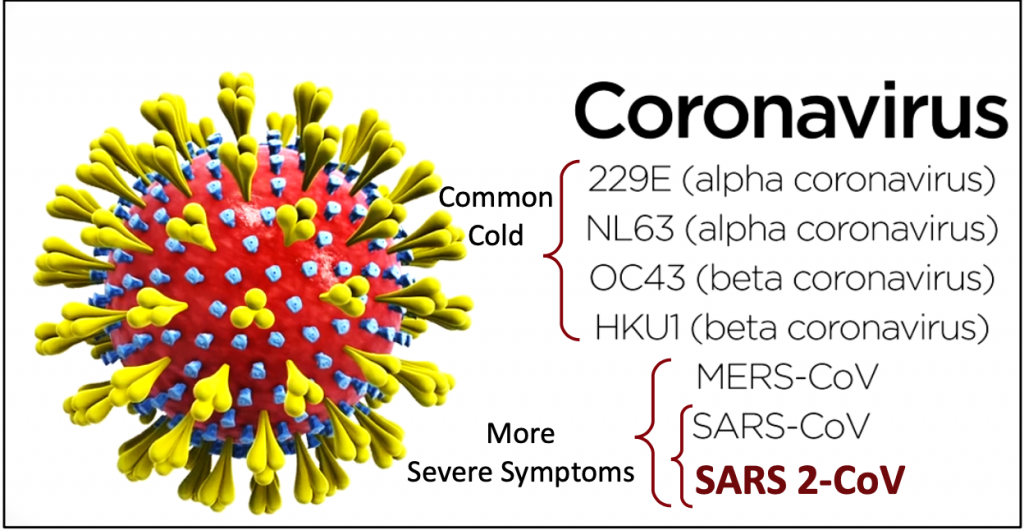
Coronavirus is a family of common respiratory viruses. There are seven different strains of coronavirus. Four can cause symptoms many people experience in the fall/winter seasons: from the common “cold” with cough and runny nose to flu-like body aches and even a low- grade fever.
SARS-1 (Severe Acute Respiratory Syndrome), MERS (Middle East Respiratory Syndrome) and most recently,SARS-2 COVID-19 are newer coronaviruses that have emerged since about 2002-2003, and may cause more serious illnesses.
Diseases that spread widely are called an epidemic if they are mostly confined to one region of the world. Pandemics refer to diseases that rapidly spread out of a region, around the world. SARS-1 first appeared in China in 2002-2003. It was classified as an epidemic, even though it spread to 26 countries. SARS 1 did spread beyond China but was not considered serious enough to be a pandemic. It had a case fatality rate of about 9.6%.
SARS-1 lasted about two seasons, and then subsided. However, because of its infectious properties, various research labs began to study the SARS-1 virus for different reasons. During these years, the virus was known to have escaped at least six times from several labs in China, causing illness outbreaks.
MERS was first reported in Saudi Arabia in 2012. Contagion reports were similar to SARS-1, but the fatality rate was much more deadly at 34.4%. MERS subsided and there have been few cases reported since the outbreak.
SARS-2 COVID-19 has been a different story. The actual infecting virus has been named SARS-2 or SARS-CoV-2 (Severe Acute Respiratory Syndrome 2) and is reported to be 79% identical to the genetic sequence of SARS 1. The name that was finally given to the “disease” is COVID-19 (short for Corona Virus Disease-2019).
SARS-2 virus and the illness, COVID 19, are classified as a pandemic because of its rapid, global spread.
Chapter 2 of a guide to home-based covid treatment
I Have Flu-Like Symptoms: What Should I Do?
What should I do first?
Consult your primary physician with the first onset of COVID-19 symptoms.
If you are experiencing severe, life threatening symptoms call 911 or go to your nearest emergency department for evaluation. Difficulty breathing or severe chest pain is a sign of serious illness and needs medical attention promptly.
The most important reason to contact your physician right away is that studies show early treatment is the KEY to success with COVID. Early treatment is especially critical for people at high-risk.
HIGH RISK PATIENTS: over age 50, with one or more other medical conditions:
- Obesity
- Diabetes, or pre-diabetes (“metabolic syndrome”)
- Lung disease (COPD, pulmonary fibrosis, asthma, cystic fibrosis)
- Kidney disease
- Hypertension
- Autoimmune disorders
- History of cancer treatment
- History of taking corticosteroids regularly
